“Almost all physicians encounter parents who refuse infant vaccines, and about 20% of pediatricians dismiss them, contrary to the 2005 American Academy of Pediatrics guideline, which was reaffirmed in 2013, according to a study published online November 2 in Pediatrics.”
Pediatrics. Published online November 2, 2015
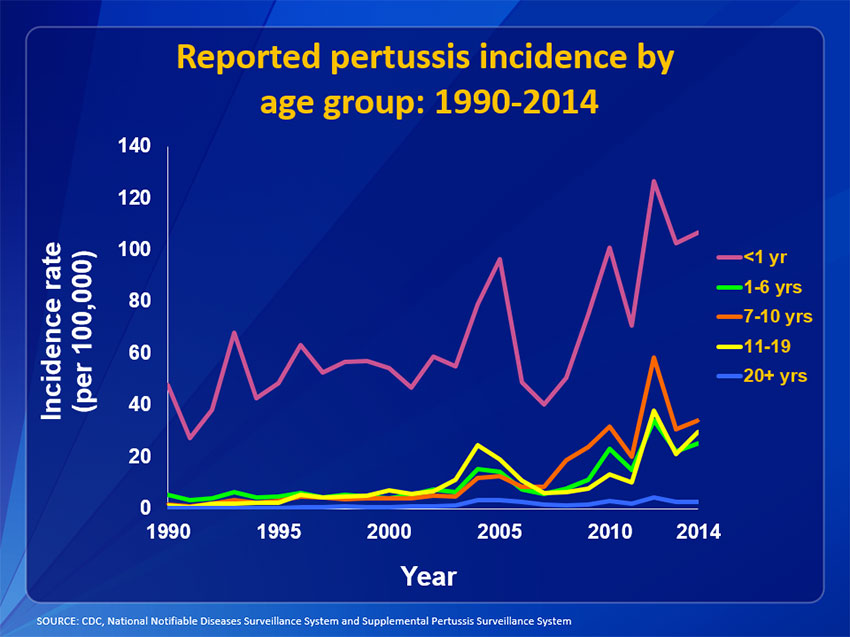
Comment: Pediatricians and other health care providers should speak to parents or expectant parents about the risk to benefit profile for each of the standard childhood vaccinations, Dtap, Ipv, Hib, HepB, Prevnar, MMR, and Varivax. There should be an opportunity for parents to openly discuss their concerns and apprehension toward vaccines. Pediatricians should provide education using a real life example such as the vaccine, Prevnar that has nearly eliminated cases of Pneumococcal meningitis that until just 20 years ago killed or severely brain devastate even the survivors. Help parents understand that there are just 2 additional vaccines added over the past couple decades. In addition the combined vaccines given to infant/children are 100 fold more pure today. Use these examples and even consider the use of the vaccine package inserts to show how the risk of the natural infection is much higher than any side effect(s) (rates are included from study patients) from each of the vaccines alone. Take a look below at what has happened to bacterial meningitis in young children since Prevnar vaccine was introduced around 2000.
From the CDC website:
CDC – Surveillance of Pneumococcal – Chapter 11 – Vaccine Preventable Diseases<!– OLD TITLE BEFORE "070711" Vaccines: Pubs/SurvManual/Pneumococcal Chapter 11 –> //www.google-analytics.com/analytics.js/TemplatePackage/js/B/jquery.js/TemplatePackage/js/B/jquery.watermark.js/TemplatePackage/js/B/common.js/TemplatePackage/js/B/startup.js/TemplatePackage/js/B/blocks-ie.js/TemplatePackage/js/B/video.js/TemplatePackage/js/B/navScripts.js/TemplatePackage/js/B/share.js/TemplatePackage/js/B/govdelivery.js/TemplatePackage/js/B/external.js/TemplatePackage/js/B/plugins.js/TemplatePackage/js/B/syndicateThisPage.js/TemplatePackage/js/B/css-include.js/TemplatePackage/js/B/socialMedia.js
/TemplatePackage/js/B/pngfix.js
/TemplatePackage/js/B/blocks-ie6.js
/TemplatePackage/js/B/jquery.curvycorners.js
/JScript/foresee/foresee-trigger.js/JScript/foresee-variables.js /TemplatePackage/js/B/socialMenu.js//search.usa.gov/javascripts/remote.loader.js/JScript/foresee/foresee-surveydef.js?build=7//search.usa.gov/assets/sayt_loader_libs.js//search.usa.gov/assets/stats.js
The following data includes cases of meningitis, blood infection, or pneumonia
“Following the introduction of PCV7 in 2000, dramatic declines in invasive pneumococcal disease were reported among children aged <5 years as early as 2001. Before introduction of PCV7, rates of PC7-type invasive pneumococcal disease among children in this age were around 80 cases per 100,000 population. After the introduction of PCV7, rates of disease due to these 7 serotypes dropped dramatically to less than 1 case per 100,000 by 2007 (Figure 1).”


 Time is of the essence, it can happen to your teenager and can take their lives away. Talk to them about vaping!
Time is of the essence, it can happen to your teenager and can take their lives away. Talk to them about vaping!



You must be logged in to post a comment.